|
|
|
Rates of testing and diagnosis are declining* and may be increasing your plan’s exposure to the high cost of osteoporosis-related fractures1,2
*Among women age 65 and over from 2009 to 2014.
|
|
|
|
Dear [Insert Customer Name],
|
|
|
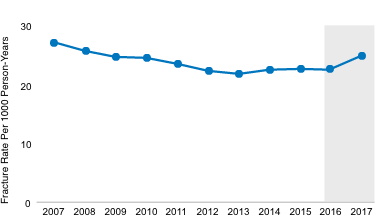
Postmenopausal osteoporosis diagnosis rates declined from 2009-2014.2 Yet, osteoporosis-related fracture rates are on the rise.3 Recent data show that total fracture rates increased beginning in 2016.3
Total Fracture in Women ≥ 65 Years of Age3,*
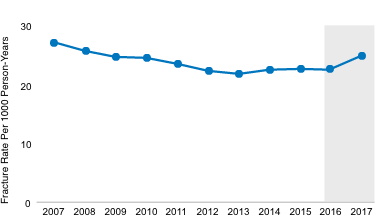
*Includes fractures of the ankle, carpal/wrist, hip, femur, pelvis, radius/ulna, shoulder, spine, tibia/fibia, or multiple sites.
|
|
|
|
|
Osteoporosis-related fractures can impact healthcare costs as much as or more than myocardial infarctions.4 Annual hospitalization costs for osteoporosis-related fractures totaled $5.1 billion compared to $4.3 billion for myocardial infarctions.4,†
|
|
|
|
|
Osteoporosis-related fractures require considerable healthcare resource utilization.5,6 Every year, there are 1.5 million osteoporosis-related fractures in the United States, leading to more than 500,000 hospital admissions.6 Among women ≥ 55 years of age, hospitalizations from 2000 to 2011 were highest for osteoporosis-related fractures when compared with myocardial infarction, stroke, and breast cancer.4
|
|
|
|
|
|
There is an 86% increased risk of a subsequent fracture after an initial fracture.7
|
|
|
|
|
|
|
This can lead to approximately twice or triple the medical cost for those who experienced a second fracture compared to those who experienced one fracture.8
|
|
|
|
|
|
|
The cost of a fracture is highest in the first year after an initial osteoporosis-related fracture and remains high in years 2 through 5.9,‡
|
|
|
|
|
With osteoporosis testing and diagnosis on the decline, osteoporosis-related fractures may lead to considerable healthcare resource utilization.1,2 Increased age- and sex-adjusted US fracture rates support the global call to action to increase screening and treatment of osteoporosis in older adults.1
|
|
|
|
Assess utilization management to ensure timely access to medications for postmenopausal osteoporosis
|
|
|
|
†Based on the total population cost for hospitalization per year for the
2000-2011 time period in women ≥ 55 years of age.
‡Costs from a study that compared direct healthcare costs between
female fracture patients (both commercially enrolled patients and
Medicare Advantage patients) and demographically matched
fracture-free patients for the 5 years after the initial fracture, by site of
fracture using claims from the IBM MarketScan® Commercial Claims
and Encounters Database (Commercial) and MarketScan® Medicare
Supplemental and Coordination of Benefits Database (Medicare).
References: 1.
1. The American Society for Bone Mineral Research. www.asbmr.org/Assets/d5139738-e1b3-4645-859a-96affc059ae3/636098972158530000/call-to-action-to-address-the-crisis-in-the-treatmentof-osteoporosisfinal-003.pdf. Accessed November 20, 2020. 2. Lewiecki EM. Abstract presented at: Annual Meeting of the American Society for Bone and Mineral Research; September 16-19, 2016; Atlanta, GA. Abstract 1077. 3. Lewiecki EM, Chastek B, Sundquist K, Williams SA, Weiss RJ, Wang Y. Osteoporotic fracture trends in a population of US managed care enrollees from 2007 to 2017. Osteoporos Int. 2020;31:1299-1304. 4. Singer A, Exuzides A, Spangler L, O’Malley C, Colby C, Johnston K, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90:53-62. 5. Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25:2359-2381. 6. U.S. Department of Health and Human Services. Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General, 2004. 7. Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375-382. 8. Song X, Shi N, Badamgarav E, Kallich J, Varker H, Lenhart G, et al. Cost burden of second fracture in the US health system. Bone. 2011;48:828-836. 9. Data on file, Amgen; 2020.
|
|
|
Amgen Inc.
One Amgen Center Drive
Thousand Oaks, CA 91320-1799
www.amgen.com
© 2020 Amgen Inc. All rights reserved.
USA-785-81449 11/20
|
|
|
|
|
|
|